Mental Health Stigma: Statistics and Definition.
“The single most important barrier to overcome in the community is the stigma and associated discrimination towards persons suffering from mental and behavioral disorders.”
The World Health Organisation
The term “stigma” originated in ancient Greece, where it was used to brand criminals or slaves. Throughout history, individuals with mental illnesses such as schizophrenia or bipolar disorder were often feared, tortured, or seen as possessed by demons. These archaic views have evolved into modern-day stigmas, which manifest as discriminatory attitudes towards those with mental health conditions.
What does stigma mean in the context of mental health? Unfortunately, myths, misunderstandings, ignorance, and negative attitudes contribute to the stigma faced by people living with mental health conditions. These individuals may be perceived as dangerous, different, or inferior. While these stigmas are neither true nor accurate, they can cause significant harm.
Mental Health Stigma: Defenition
Stigma is a negative and often unfair social attitude attached to a person or group, often placing shame on them for a perceived deficiency or difference. Once established, stigmas can be challenging to dismantle and overcome. They can affect individuals based on their way of life, cultural beliefs, lifestyle choices, or health conditions, including mental illnesses.
Harmful Effects Of Stigma Include:
- Bullying, physical violence, or harassment
- Lack of understanding from family, friends, co-workers, or others
- Fewer opportunities for work, school, or social activities
- Reluctance to seek help or treatment
- Inadequate health insurance coverage for mental illness treatment
- The belief that success is unattainable due to their condition
Mental Health Stigma: Statistics
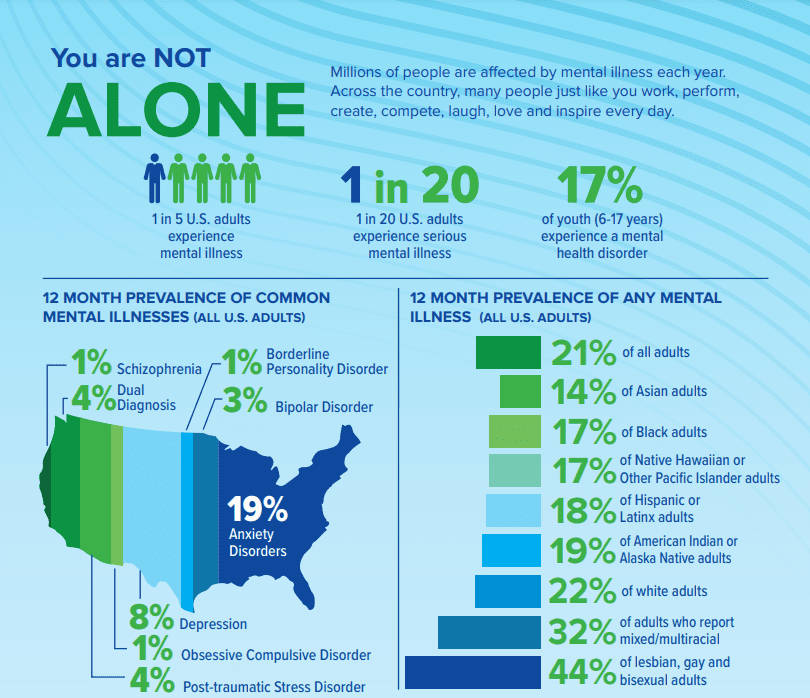
Millions of people in the U.S. are affected by mental illness. These numbers provided in this article are a powerful tool for raising public awareness and advocating for better health care.
- 1 in 5 U.S. adults experience mental illness each year
- 1 in 20 U.S. adults experience serious mental illness each year
- 1 in 6 U.S. youth aged 6-17 experience a mental health disorder each year
- 50% of all lifetime mental illness begins by age 14, and 75% by age 24
- Suicide is the 2nd leading cause of death among people aged 10-34
You Are Not Alone
- 20.6% of U.S. adults experienced mental illness in 2019 (51.5 million people). This represents 1 in 5 adults.
- 5.2% of U.S. adults experienced serious mental illness in 2019 (13.1 million people). This represents 1 in 20 adults.
- 16.5% of U.S. youth aged 6-17 experienced a mental health disorder in 2016 (7.7 million people)
- 3.8% of U.S. adults experienced a co-occurring substance use disorder and mental illness in 2019 (9.5 million people)
- Annual prevalence of mental illness among U.S. adults, by demographic group:
- Non-Hispanic Asian: 14.4%
- Non-Hispanic white: 22.2%
- Non-Hispanic black or African-American: 17.3%
- Non-Hispanic American Indian or Alaska Native: 18.7%
- Non-Hispanic mixed/multiracial: 31.7%
- Non-Hispanic Native Hawaiian or Other Pacific Islander: 16.6%
- Hispanic or Latino: 18.0%
- Lesbian, Gay or Bisexual: 44.1%
- Annual prevalence among U.S. adults, by condition:
- Major Depressive Episode: 7.8% (19.4 million people)
- Schizophrenia: <1% (estimated 1.5 million people)
- Bipolar Disorder: 2.8% (estimated 7 million people)
- Anxiety Disorders: 19.1% (estimated 48 million people)
- Posttraumatic Stress Disorder: 3.6% (estimated 9 million people)
- Obsessive Compulsive Disorder: 1.2% (estimated 3 million people)
- Borderline Personality Disorder: 1.4% (estimated 3.5 million people)
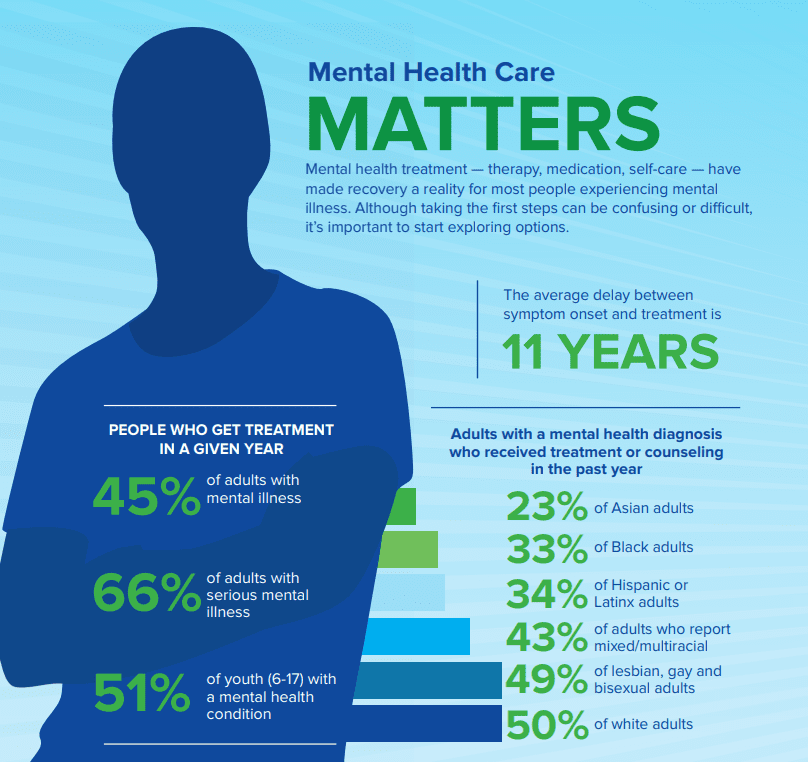
Mental Health Care Matters
- 44.8% of U.S. adults with mental illness received treatment in 2019
- 65.5% of U.S. adults with serious mental illness received treatment in 2019
- 50.6% of U.S. youth aged 6-17 with a mental health disorder received treatment in 2016
- The average delay between onset of mental illness symptoms and treatment is 11 years
- Annual treatment rates among U.S. adults with any mental illness, by demographic group:
- Male: 36.8%
- Female: 49.7%
- Lesbian, Gay or Bisexual: 49.2%
- Non-Hispanic Asian: 23.3%
- Non-Hispanic white: 50.3%
- Non-Hispanic black or African-American: 32.9%
- Non-Hispanic mixed/multiracial: 43.0%
- Hispanic or Latino: 33.9%
- 10.9% of U.S. adults with mental illness had no insurance coverage in 2019
- 11.9% of U.S. adults with serious mental illness had no insurance coverage in 2019
- 55% of U.S. counties do not have a single practicing psychiatrist
The Ripple Effect Of Mental Illness
PERSON:
- People with depression have a 40% higher risk of developing cardiovascular and metabolic diseases.
- 18.4% of U.S. adults with mental illness also experienced a substance use disorder in 2019.
- The unemployment rate is higher among U.S. adults with mental illness (5.8%) compared to those without (3.6%).
- High school students with significant symptoms of depression are more than twice as likely to drop out compared to their peers.
FAMILY:
- At least 8.4 million people in the U.S. provide care to an adult with a mental or emotional health issue.
- Caregivers of adults with mental or emotional health issues spend an average of 32 hours per week providing unpaid care.
COMMUNITY:
- Mental illness and substance use disorders are involved in 1 out of every 8 emergency department visits by U.S. adults.
- Mood disorders are the most common cause of hospitalization for people under age 45 (excluding pregnancy and birth-related hospitalizations).
- Severe mental illness causes $193.2 billion in lost earnings each year.
- 20.5% of people experiencing homelessness in the U.S. have a serious mental health condition.
- 37% of adults incarcerated in the state and federal prison system have a diagnosed mental illness.
- 70.4% of youth in the juvenile justice system have a diagnosed mental illness.
- 41% of Veteran’s Health Administration patients have a diagnosed mental illness or substance use disorder.
WORLD:
- Depression and anxiety disorders cost the global economy $1 trillion in lost productivity each year.
- Depression is a leading cause of disability worldwide.
It’s Okay To Talk About Suicide
- Suicide is the 2nd leading cause of death among people aged 10-34 in the U.S.
- Suicide is the 10th leading cause of death in the U.S.
- The overall suicide rate in the U.S. has increased by 35% since 1999
- 46% of people who die by suicide had a diagnosed mental health condition
- 90% of people who die by suicide have shown symptoms of a mental health condition, according to interviews with family, friends, and medical professionals (also known as psychological autopsy)
- Lesbian, gay, and bisexual youth are 4x more likely to attempt suicide than straight youth.
- 78% of people who die by suicide are male
- Transgender adults are nearly 12x more likely to attempt suicide than the general population
- Annual prevalence of serious thoughts of suicide by U.S. demographic group:
- 4.8% of all adults
- 11.8% of young adults aged 18-25
- 18.8% of high school students
- 46.8% of lesbian, gay, and bisexual high school students
If you or someone you know is in an emergency, call The National Suicide Prevention Lifeline at 800-273-TALK (8255) or call 911 immediately. If you are searching for treatment
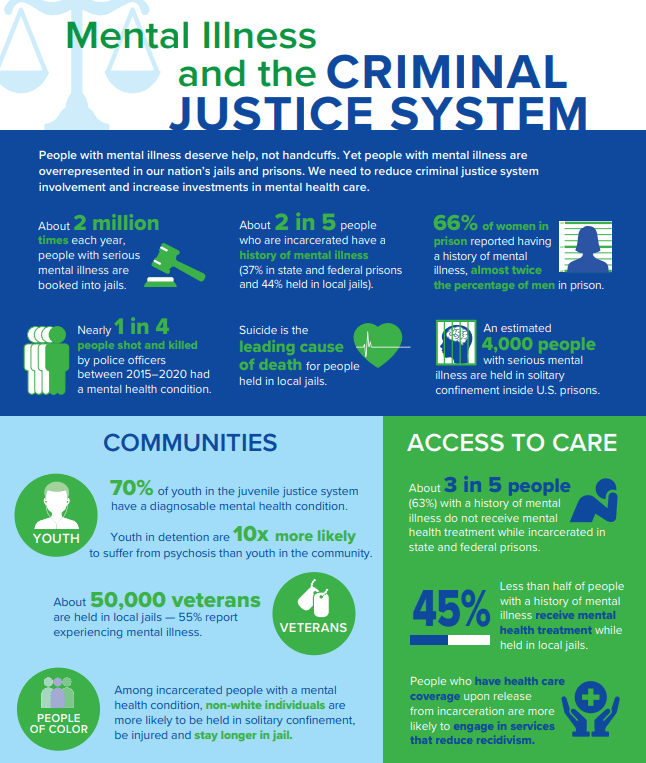
Mental Illness And The Criminal Justice System
CRIMINAL JUSTICE SYSTEM
- About 2 million times each year, people with serious mental illness are booked into jails.
- About 2 in 5 incarcerated individuals have a history of mental illness (37% in state and federal prisons and 44% in local jails).
- 66% of women in prison reported having a history of mental illness, nearly twice the percentage of men.
- Nearly one in four people shot and killed by police officers between 2015 and 2020 had a mental health condition.
- Suicide is the leading cause of death for people held in local jails.
- An estimated 4,000 people with serious mental illness are held in solitary confinement in U.S. prisons.
Access to care:
- About 3 in 5 people with a history of mental illness do not receive mental health treatment while incarcerated in state and federal prisons.
- Less than half of those with a history of mental illness receive mental health treatment while held in local jails.
- People with healthcare coverage upon release from incarceration are more likely to engage in services that reduce recidivism.
Ways to Fight Mental Health Stigma
Most people who live with mental illness have, at some point, been blamed for their condition. They might have been called names, or their symptoms might have been referred to in offensive ways. They have been illegally discriminated against, with no justice. This is the power that stigma holds. Stigma causes people to feel ashamed for something out of their control. Worst of all, stigma prevents people from seeking the help they need because they are embarrassed. For people who already carry such a heavy burden of the illness itself, stigma is an unacceptable addition to their pain. And while stigma has reduced in recent years, progress has not been quick enough.
Most people with mental illness have, at some point, been blamed for their condition. They might have been called names or had their symptoms referred to in offensive ways. They have been illegally discriminated against, with no justice. This is the power of stigma. It causes people to feel ashamed for something that is out of their control and prevents them from seeking the help they need. For those already carrying the heavy burden of the illness itself, stigma adds an unacceptable layer of pain. While stigma has reduced in recent years, progress has been slow.
The mental health community needs to raise its voice against stigma. Here are several ways to do so:
- Get the mental health treatment you need. Do not let the fear of being labeled stop you from getting help. Do not define yourself by your illness. For example, say “I have schizophrenia” instead of “I’m schizophrenic.”
- Talk openly about mental health. Sharing your story encourages others to learn about and accept mental health conditions.
- Educate yourself and others about mental health. Challenge stereotypes and misconceptions respectfully.
- Be conscious of language. Avoid using stigmatizing words like “crazy” or “psycho.”
- Encourage equality between physical and mental illness. Speak of mental illness in the same terms as physical illnesses.
- Show compassion for those with mental illness. Learn more about their experiences and backgrounds.
- Let the media know when they’re being stigmatized. Speak out against simplified explanations of nuanced problems that rely on stigmatizing people with mental illness.
.
Statistics and infographics provided by NAMI at https://www.nami.org/mhstats

At Overland Intensive Outpatient, our philosophy is to help treat mental health by uncovering the underlying causes and addressing the co-occurring disorders which could drive the individual to relapse. We understand that every person who enters our doors comes with unique needs and goals. Our experienced clinicians will work one-on-one with clients to develop a comprehensive treatment plan using evidence-based methods. Overland Intensive Outpatient is ready to provide both in-person and virtual care (telehealth services) to expand access to essential health services and meet the health needs of our patients. If you need FREE help please contact the National Helpline about mental and/or substance use disorders, prevention, treatment, and recovery in English and Spanish.
Published: December 23, 2021

Published: February 14, 2026
Medication-Assisted Treatment (MAT): How It Works?
Summary: Medication-assisted treatment (MAT) is an evidence-based approach to addiction treatment that combines FDA-approved medications with behavioral therapy and counseling to treat substance use disorders — primarily opioid and alcohol addiction. MAT is endorsed by the Substance Abuse and Mental Health Services Administration (SAMHSA), the National Institute on Drug Abuse (NIDA), and the World Health […]
Read more
Published: February 06, 2026
Talk Therapy: Types, Benefits & How It Works in California
Summary: Talk therapy — also known as psychotherapy — is a structured, evidence-based treatment approach in which a trained mental health professional helps individuals identify, understand, and change the thoughts, emotions, and behaviors that contribute to mental health conditions and substance use disorders. It is the foundation of treatment for depression, anxiety, PTSD, personality disorders, […]
Read more
Published: January 27, 2026
What Is DPD? Understanding Dependent Personality Disorder
Most people don’t ask, “What is DPD or Dependent Personality Disorder?” They come in feeling drained, anxious, and stuck in relationships that feel restrictive yet hard to leave. Being alone feels unsettling. Decision-making feels paralyzing. Reassurance becomes a daily necessity rather than a comfort. At Overland IOP in Los Angeles, we often see Dependent Personality […]
Read more
