Suicidal Ideation: Facts, Risk Factors, Warning Signs and Treatment
According to National Survey by the Substance Abuse and Mental Health Services Administration, 4.3% of U.S. adults ages 18 and older had thoughts about suicide.
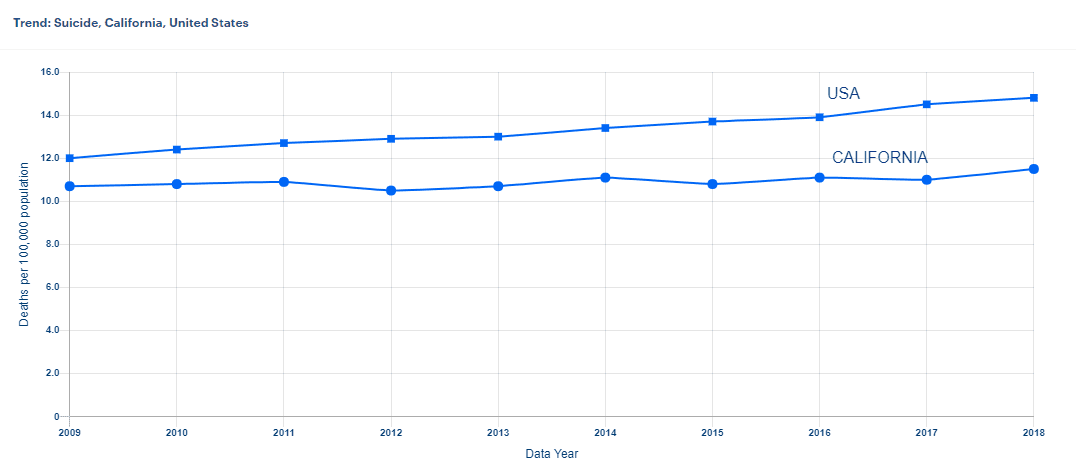
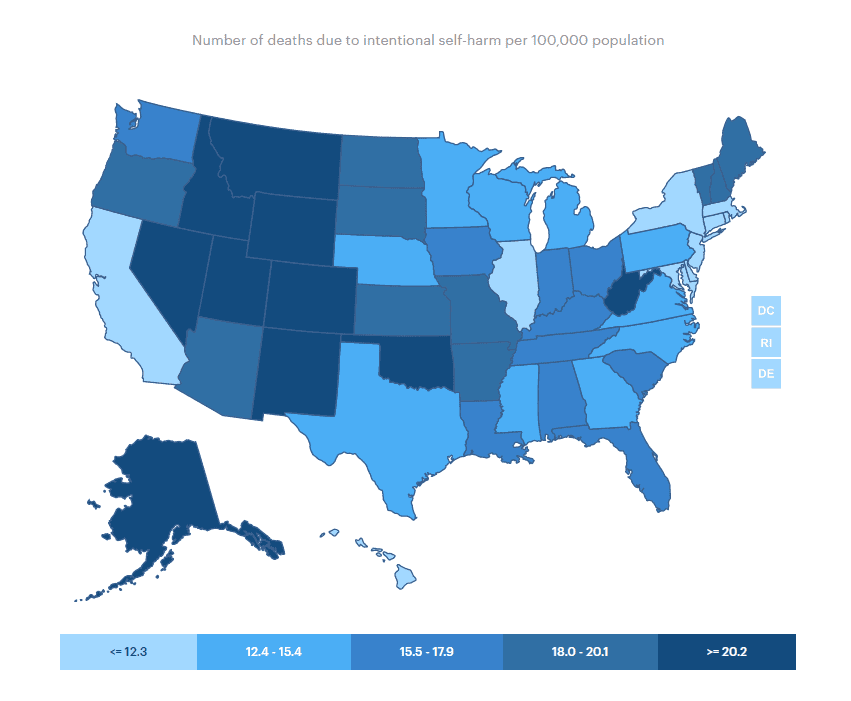
Unfortunately, suicides are on the rise. According to the Centers for Disease Control and Prevention, half of the states in the United States report more than a 30% increase since 1999, and nearly all the rest reporting increased rates since then.
For people with mental health disorders, this rate is significantly higher. Again, the exact numbers are unclear, but since suicidal ideation is a symptom of mental health disorders like depression, bipolar disorder, mood disorders, schizophrenia, anxiety, and certain personality disorders, the problem exists at a far greater percentage when it comes to people with mental health disorders.
With all that being said, understanding the issues concerning suicide and mental health is an important way to take part in suicide prevention, help others in crisis, and change the conversation around suicide. If you have suicidal thoughts, contact the National Suicide Prevention Lifeline at 1-800-273-8255 for support and assistance from a trained counselor. If you or a loved one are in immediate danger, call 911.
What Is Suicidal Ideation?
“Suicidal ideations,” often called “suicidal thoughts,” is a broad term used to describe a range of contemplations, wishes, and preoccupations with death and suicide.
Suicidal ideation is one of the symptoms of depression, bipolar disorder, schizophrenia, anxiety, but it may also occur in people with other mental illnesses or no mental illness at all.
Not everyone with suicidal ideation acts on it. There are two kinds of suicidal ideation: passive and active. Passive suicidal ideation occurs when you wish you were dead or that you could die, but you don’t actually have any plans to commit suicide.
Active suicidal ideation, on the other hand, is not only thinking about it but having the intent to commit suicide, including planning how to do it. If you or a loved one has passive or active suicidal ideation, you should get help right away.
Suicidal Ideation: Risk Factors
Things that can make you more likely to have suicidal ideation include:
- Mental disorders, particularly mood disorders, schizophrenia, anxiety disorders, and certain personality disorders
- Alcohol and other substance use disorders
- Hopelessness
- Impulsive and/or aggressive tendencies
- History of trauma or abuse
- Major physical illnesses
- Previous suicide attempt
- Family history of suicide
- Job or financial loss
- Loss of relationship
- Easy access to lethal means
- Local clusters of suicide
- Lack of social support and sense of isolation
- Stigma associated with asking for help
- Lack of healthcare, especially mental health and substance abuse treatment
- Cultural and religious beliefs, such as the belief that suicide is a noble resolution of a personal dilemma
- Exposure to others who have died by suicide (in real life or via the media and Internet)
Suicidal Ideation: Warning Signs
Some warning signs may help you determine if you or a loved one is at risk for suicide, especially if the behavior is new, has increased, or seems related to a painful event, loss, or change. If you or someone you know exhibits any of these, seek help ASAP:
- Talking about wanting to die or to kill themselves
- Looking for a way to kill themselves, like searching online or buying a gun
- Talking about feeling hopeless or having no reason to live
- Talking about feeling trapped or in unbearable pain
- Talking about being a burden to others
- Increasing the use of alcohol or drugs
- Acting anxious or agitated; behaving recklessly
- Sleeping too little or too much
- Withdrawing or isolating themselves
- Showing rage or talking about seeking revenge
- Extreme mood swings

Suicidal Ideation: Treatment
As we already mentioned in this article, suicide is the 10th leading cause of death in the United States and the 2nd leading cause of death in people between the ages of 10-34. The gravity of the situation can be seen in the fact that every 11 minutes, one person loses their life to suicide. What is worse, many cases of suicide are not even reported due to stigma, religious beliefs, and other concerns. Hence, the actual picture may be even darker than statistics shows.

What if You’re Worried About a Loved One?
If you’re concerned that someone you care about might have suicidal ideation:
Have a candid talk. Ask them: “Are you thinking about killing yourself?” Experts say that as hard as it is to ask this won’t make your loved one think about suicide more.
Show support. Research says talking about it and acknowledging it may help your loved one think about suicide less often.
Find support. Add the National Suicide Prevention Lifeline — 800-273-TALK (8255) — and the Crisis Text Line’s number (741741) to your phone contacts. Share these numbers with your loved one, too. If the risk of suicide is mild or moderate you could also connect with an outpatient mental health treatment center, like Overland in Los Angeles, California.
Stay in touch. Check-in with them often after you talk. Let them know you’re there for them when they need you.


Overland is the top-rated mental health, addiction, and codependency treatment center in Los Angeles, California. We provide IOP, PHP programs and in-person, virtual care (telehealth services), hybrid treatment plans.
If you or your loved one have suicidal thoughts, but there is no crisis, you might benefit from an IOP or PHP program that can help reduce the risk of suicide. Inpatient hospital care might recommend this if you or your loved one think about suicide often and if the thoughts last a long time or include a suicidal plan to die by suicide.
Contact Overland IOP today via phone, live chat, contact forms, or email! We work 24/7 and provide in-person, virtual care (telehealth services), and hybrid treatment plans. Our IOP and PHP programs offer morning, afternoon, or evening options. Start your treatment as soon as the same day!
Published: November 18, 2021

Published: February 14, 2026
Medication-Assisted Treatment (MAT): How It Works?
Summary: Medication-assisted treatment (MAT) is an evidence-based approach to addiction treatment that combines FDA-approved medications with behavioral therapy and counseling to treat substance use disorders — primarily opioid and alcohol addiction. MAT is endorsed by the Substance Abuse and Mental Health Services Administration (SAMHSA), the National Institute on Drug Abuse (NIDA), and the World Health […]
Read more
Published: February 06, 2026
Talk Therapy: Types, Benefits & How It Works in California
Summary: Talk therapy — also known as psychotherapy — is a structured, evidence-based treatment approach in which a trained mental health professional helps individuals identify, understand, and change the thoughts, emotions, and behaviors that contribute to mental health conditions and substance use disorders. It is the foundation of treatment for depression, anxiety, PTSD, personality disorders, […]
Read more
Published: January 27, 2026
What Is DPD? Understanding Dependent Personality Disorder
Most people don’t ask, “What is DPD or Dependent Personality Disorder?” They come in feeling drained, anxious, and stuck in relationships that feel restrictive yet hard to leave. Being alone feels unsettling. Decision-making feels paralyzing. Reassurance becomes a daily necessity rather than a comfort. At Overland IOP in Los Angeles, we often see Dependent Personality […]
Read more
